Alzheimer’s disease (AD) was first identified over a century ago and has since grown into a major global health challenge. In 1906, a German psychiatrist named Alois Alzheimer described a patient with profound memory loss and confusion, marking the first recognition of this “peculiar disease”[Link]. A few years later, the illness was officially named “Alzheimer’s disease” in his honor [Link]. Back then it was a rare curiosity; today, AD affects tens of millions worldwide, reflecting an alarming rise, especially in the last 30 years with earlier and earlier diagnosis.
For example, the number of people living with dementia globally jumped from about 20 million in 1990 to over 43 million by 2016 [Link]. This dramatic increase makes AD one of the most prevalent and costly neurodegenerative diseases of our time. In short, what began as a single case study in the early 1900s has become a defining environmentally caused public health issue of the 21st century.
Deeper Historical Context and Trends
Alois Alzheimer’s first patient, a 51-year-old woman named Auguste D., exhibited memory problems, disorientation, and behavioral changes that puzzled doctors [Link] and [Link]. After her death, Dr. Alzheimer examined her brain tissue and noted distinctive abnormalities clumps and tangled fibers – which he reported in November 1906 as “a peculiar severe disease process of the cerebral cortex” [Link]. His findings initially drew little interest[Link], but eminent psychiatrist Emil Kraepelin was impressed and in 1910 named the illness Alzheimer’s disease in the 8th edition of his psychiatry textbook[Link]. Alzheimer went on to document a few more cases before his untimely death in 1915[Link].
Over subsequent decades, what we now call Alzheimer’s disease was recognized as the most common cause of dementia in older adults. Historically, it was often misattributed to “senility” or normal aging, but work by Alzheimer and others showed it to be a distinct pathological entity. Prevalence has soared in recent times due to aging populations. For instance, worldwide dementia cases increased by roughly 117% from 1990 to 2016 alone[Link]. In the United States, an estimated 6.9 million people age 65 and older are living with Alzheimer’s in 2024, compared to only a few million a few decades ago [Link] and [Link]. Improved awareness and diagnosis also contribute to higher reported numbers. Unfortunately, Alzheimer’s has also climbed the ranks of leading causes of death; it is currently the 6th leading cause of death in the U.S. (and the 5th among those over 65)[Link]. No cure by centralized medicine has been found yet, but the accumulation of knowledge since Alois Alzheimer’s discovery has laid the foundation for modern research into causes, prevention, and treatment. And through a biophysics lens we propose a way to prevent, slow and potentially even reverse the condition.
Key Historical Points
-
First Case: Auguste D., examined by Alois Alzheimer in 1901–1906, showing memory loss, paranoia, and disorientation[Link].
-
First Report: November 3, 1906 – Alzheimer presents the case’s neuropathology (plaques and tangles) to colleagues[Link].
-
Naming: 1910 – Emil Kraepelin names it “Alzheimer’s disease” in a medical text[Link].
-
Prevalence Growth: ~20 million cases globally in 1990 vs. 55+ million today[Link] and [Link], driven by longer lifespans and better recognition.
-
Modern Era: Now understood as a distinct disease process causing dementia, subject to intensive research and increasingly urgent public health measures.
Hallmark Pathology and Underlying Biophysical Mechanisms
Alzheimer’s disease is defined by two signature features in the brain: amyloid plaques and tau tangles. Amyloid plaques are sticky clumps of protein fragments (called beta-amyloid) that build up between neurons, while tau tangles are twisted fibers of a protein (tau) that form inside neurons[Link]. These plaques and tangles, first observed by Alois Alzheimer in his patient’s brain, disrupt how brain cells work. Think of plaques as gumming up the spaces between cells and tangles as choking the cells from within. Over time, their accumulation leads to the death of brain cells and the characteristic memory loss and cognitive decline of AD. However, scientists now know that these protein deposits are just the tip of the iceberg. Beneath the plaques and tangles lies a web of biophysical processes that go wrong – involving the energy factories of cells (mitochondria), the balance of oxidation in cells, the water environment surrounding proteins, and even subtle electrical or light-based signals in cells. In this section, we first explain the classic plaques and tangles, then delve into these deeper biophysical mechanisms that precede and promote the protein buildup.
Beta-amyloid plaques (brown clumps outside neurons) and tau tangles (bluish threads inside neurons) are the classic microscopic lesions of Alzheimer’s disease[Link].

Figure: ikimedia Commons. (2017). Beta-amyloid plaques and tau in the brain [Image]. Retrieved from https://commons.wikimedia.org/wiki/File:Beta-Amyloid_Plaques_and_Tau_in_the_Brain_(38686503251).png#:~:text=In%20the%20Alzheimer%E2%80%99s%20affected%20brain%2C,a%20tipping%20point%2C%20there%20is
In this NIH illustration, amyloid plaques crowd around neurons, disrupting cell-to-cell signaling, while tau protein has formed tangles within the neurons (visible as knotted fibers inside the blue-stained cell bodies). These protein aggregates gradually spread through the brain’s memory and thinking centers. Modern research suggests that such aggregates result from a complex cascade of underlying processes including oxidative stress, metabolic dysfunction, and other factors that begin years before plaques and tangles become widespread.
Hallmark Plaques and Tangles (Central Dogma of AD Pathology)
By mid-20th century, researchers established that extracellular beta-amyloid plaques and intracellular neurofibrillary tangles are the defining histological features of AD[Link]. Beta-amyloid (Aβ) plaques form when a larger protein (APP) is cut into fragments that misfold and stick together in the brain tissue[Link]. These plaques collect in the spaces between neurons, interfering with cell communication. Tau tangles, on the other hand, form inside neurons from a normal cell-stabilizing protein called tau that becomes abnormally hyperphosphorylated and twists into filaments[Link]. Tangles clog the internal transport system of neurons and lead to cell dysfunction and death. The amyloid and tau pathologies often start in specific brain regions (explained more in Section 3) and then spread. For decades, the dominant “amyloid cascade hypothesis” held that amyloid accumulation is the initial trigger of AD, setting off tau tangles and cell death [Link]. Indeed, rare genetic forms of AD (familial AD) involve mutations in genes related to amyloid production, causing early plaque buildup. However, emerging evidence suggests a more complex interplay: amyloid and tau pathologies likely influence each other and are accelerated by broader cellular problems[Link]. In other words, plaques and tangles are crucial markers, but they arise from a convergence of underlying biophysical breakdowns. Research now is intensely focused on those upstream factors, oxidative stress, mitochondrial failure, protein misfolding dynamics, etc., to understand why plaques and tangles form in the first place.
Subcellular Redox Imbalance and Protein Misfolding
Long before a neuron is filled with tangles or surrounded by plaques, it often undergoes chronic oxidative stress and redox (reduction-oxidation) imbalance. The brain is an energy-intensive organ and produces a lot of reactive oxygen species (ROS) as by-products of metabolism. In a healthy cell, antioxidants and efficient metabolism keep ROS in check. In AD, this balance falters whether due to age, genetic susceptibility, or environmental insults leading to excess oxidative damage to proteins, lipids, and DNA in the neuron[Link]. Oxidative stress can cause proteins like amyloid and tau to misfold or accumulate. For example, ROS can directly modify the amyloid precursor protein processing or impair the protein quality-control systems, tipping the scales toward plaque formation. Neurons under redox imbalance often have damaged chaperone proteins and proteasomes, so misfolded proteins aren’t refolded or degraded properly. This creates a snowball effect: misfolded proteins beget more misfolding (a kind of chain reaction), eventually yielding the large aggregates we recognize as plaques and tangles. In fact, prion-like propagation of misfolded proteins is now a key concept: once some proteins misfold into the toxic beta-sheet-rich shapes, they can induce neighboring normal proteins to misfold in the same way, spreading the pathology through the brain[Link]. Both amyloid-β and tau have been shown in laboratory models to self-propagate like prions, meaning the misfolded form acts as a “seed” that converts other molecules and transmits to new brain areas over time[Link]. Thus, an initial redox-induced misfolding event in one region (say, the hippocampus) can eventually lead to widespread plaque/tangle pathology.
Role of Interfacial Water and Protein Folding Dynamics
Every protein in our cells, including amyloid and tau, is surrounded by a layer of water molecules. This interfacial water is not just passive solvent, it plays an active role in how proteins fold and interact [Link]. Biophysicists suggest that water in cells can exist in more ordered, structured states (sometimes called coherent domains or “structured water”) versus disordered, chaotic states. Ordered water networks can stabilize proteins and help them maintain their correct shape[Link]. Studies confirm that high-quality ordered water around proteins significantly increases protein stability and proper folding rate [Link]. On the other hand, when the cellular water environment becomes disordered, due to dehydration, excess heat, or chemical perturbants, proteins are more prone to misfold and aggregate. In AD, factors like chronic inflammation or high glucose can lead to cellular dehydration or altered water structuring, thereby impairing protein folding homeostasis. Additionally, an intriguing factor is deuterium, a heavy isotope of hydrogen present in water. Although naturally only ~0.015% of hydrogen atoms are deuterium, researchers in quantum biology propose that even this small fraction can impact biology. Normally, our mitochondria and peroxisomes help deplete deuterium from metabolic water, keeping it away from sensitive structures [Link]. if deuterium levels build up (through diet or metabolic dysfunction), it can get incorporated into water and organic molecules in place of normal hydrogen. Because deuterium is twice as heavy, bonds involving it are stronger and chemical reactions (like enzymes folding proteins or producing ATP) run slower [Link]. In essence, excess deuterium can disrupt the “structured water” networks and hamper enzymes. In the context of AD, a high deuterium load could further reduce mitochondrial ATP output and promote protein aggregation. Indeed, it’s been hypothesized that a breakdown in the natural deuterium exclusion by mitochondria leads to lower energy production and more oxidative stress, creating conditions ripe for amyloid/tau misfolding [Link]. While this deuterium aspect is a newer hypothesis, it underscores the importance of the water environment and subtle quantum-level factors in AD biophysics.
Mitochondrial Dysfunction and Bioenergetic Failure
Mitochondria, the energy powerhouses of cells, are at the center of many AD theories. Neurons rely heavily on mitochondria to generate ATP (energy currency) and to regulate cellular calcium and ROS. In early AD, neurons often show a drop in mitochondrial efficiency and signs of damage to mitochondrial DNA and membranes[Link][Link]. A leading hypothesis (the “mitochondrial cascade hypothesis”) posits that in sporadic late-life AD, mitochondrial dysfunction is an initial trigger: as one ages, mitochondrial DNA mutations accumulate and oxidative phosphorylation becomes less efficient, leading to energy shortages and high ROS in neurons[Link]. Low ATP means the neuron’s protein-folding chaperones and clearance systems (like ubiquitin-proteasome and autophagy) do not work well (they all require energy), so misfolded proteins start to pile up[Link]. High ROS, as mentioned, directly damages proteins and promotes amyloidogenic processes. Furthermore, impaired mitochondria release pro-apoptotic factors and can initiate cell death pathways. Research has shown that amyloid and tau pathologies themselves can further damage mitochondria, creating a vicious cycle, but importantly, mitochondrial issues often precede significant plaque/tangle accumulation in many patients[Link]. For example, brain imaging studies of people at risk for AD (with family history or mild impairment) show reduced glucose utilization (a sign of metabolic slowdown) in certain brain areas years before clinical symptoms. This is essentially “energy failure” in the brain, a reason AD is sometimes described as a type of metabolic disease (more on the “Type 3 diabetes” concept below). On the electrical side, mitochondria also help maintain the delicate charge balance across neuronal membranes. When their function declines, neurons may become less electrically stable and less able to generate signals properly, contributing to cognitive dysfunction even before neurons die. In summary, malfunctioning mitochondria set the stage for AD by weakening the neuron’s ability to handle normal proteins and stresses; this leads to misfolded proteins (that become plaques and tangles) and ultimately to synaptic loss and cell death[Link]. Efforts to boost mitochondrial health and restore redox balance are therefore viewed as promising strategies to slow or prevent Alzheimer pathology.
Biophotonic Signals and Cellular Distress
One of the more fascinating biophysical aspects of cells is that they emit extremely weak light known as ultra-weak photon emissions or biophotons. Neurons, being highly active cells, continuously produce low-level biophotonic signals across a broad spectrum (UV to infrared) as a by-product of metabolic and oxidative processes[Link]. Under normal conditions, this glow is minimal and likely serves some signaling roles. Under stress, however, cells can emit bursts of photons, essentially light, due to excited molecules relaxing or reactions like lipid peroxidation. In Alzheimer’s disease and other neurodegenerative conditions, scientists have observed altered biophoton emission patterns that correlate with disease activity[Link][Link]. For instance, a rodent study found that AD-model rats (induced by a toxin to mimic sporadic AD) showed increased spontaneous photon emission from the hippocampus, corresponding with high oxidative stress in that region[Link]. When those rats were treated with an AD drug (donepezil), both the oxidative stress markers and the excessive photon emissions reduced[Link].
This suggests that neurons may literally “shine” under distress, and measuring this could be a novel way to monitor AD progression. Biophotons might also play a role in cell-to-cell communication: some researchers hypothesize that neurons could use photons in addition to electrical and chemical signals (though this is still speculative). In AD, as misfolded proteins accumulate and mitochondrial dysfunction worsens, the affected cells likely experience high metabolic strain, which could manifest as aberrant biophoton release. It’s even been proposed to develop photonic biosensors to detect such signals for early diagnosis[Link][Link]. Whether biophoton bursts contribute to pathology (perhaps by inducing neighboring cells to stress) or are merely a by-product is not yet clear. But they certainly reflect the underlying redox state of the brain, brighter emission indicating greater oxidative stress and metabolic imbalance[Link]. Thus, AD brains might be “noisy” not just in electrical terms but also in a photonic sense, giving us another window into the biophysics of the disease.
Glucose, Insulin, and “Type 3 Diabetes” in the Brain
Another critical layer of Alzheimer’s biophysics involves how the brain handles glucose and insulin. The brain normally consumes glucose as its primary fuel, and insulin plays roles in neuronal signaling and glucose regulation. In many AD patients, especially sporadic late-onset cases, the brain develops a resistance to insulin and a deficiency in insulin signaling. This has led some researchers to nickname Alzheimer’s disease “Type 3 diabetes”, essentially, diabetes of the brain[Link]. Just as in type 2 diabetes the body’s cells become insulin-resistant, in AD the neurons become less responsive to insulin and have impaired glucose uptake and metabolism.
This cerebral insulin resistance is evidenced by reduced insulin receptors and signaling activity in postmortem AD brains and by imaging studies showing lower glucose utilization (hypometabolism) in AD-affected brain regions. The consequences of insulin resistance in the brain are far-reaching: insulin normally helps neurons survive and modulate neurotransmitters, so its loss makes neurons vulnerable. Moreover, insulin-degrading enzyme (IDE) is one of the main enzymes that breaks down insulin and beta-amyloid. If the brain is flooded with insulin (from insulin resistance), IDE gets tied up degrading insulin and cannot clear amyloid efficiently, leading to faster plaque buildup[Link]. Hyperinsulinemia (high insulin) thus saturates the amyloid clearance mechanism, linking peripheral metabolic dysfunction to AD pathology[Link].
Additionally, high blood sugar and its by-products (advanced glycation end-products) can directly damage proteins and mitochondria, contributing to the redox imbalance mentioned above. The term Type 3 diabetes is not meant to imply that AD is literally diabetes, but it underscores a key point: the brain’s energy metabolism is broken in AD. Decades before dementia, many individuals with AD pathology show decreased cerebral metabolic rates. Insulin resistance in the brain can also exacerbate tau pathology; studies indicate that insulin signaling helps keep tau from aggregating, so when signaling is low, tau is more likely to form tangles. In summary, Alzheimer’s can be seen as a metabolic disease of the brain where neurons are essentially starving in the midst of plenty, glucose may be abundant, but they can’t use it effectively. This insight has driven research into insulin-sensitizing drugs, intranasal insulin, and ketogenic diets for cognitive impairment (since ketones can fuel brain cells when glucose cannot see Section 4). Managing brain insulin resistance and blood sugar levels is increasingly recognized as vital in addressing the biophysical root causes of AD[Link][Link].
Environmental Factors: Light, EMFs, and Circadian Disruption
Our modern environment exposes us to unnatural stimuli that can perturb the brain’s biophysical equilibrium. Two notable factors are excess blue light and artificial electromagnetic fields (EMFs). High-energy visible light (HEVL), especially blue wavelengths (~450–480 nm) emitted by LEDs, screens, and bulbs, can disrupt circadian rhythms when used at night. Humans evolved with bright blue-rich light only during daytime (from the sun) and darkness with warm firelight at night. Constant exposure to blue light after sunset (through phones, TVs, lighting) suppresses melatonin, a hormone that not only regulates sleep but is also a potent neural antioxidant and amyloid-clearance promoter[study]. Chronic circadian disruption for example, due to late-night light exposure or irregular sleep schedules, has been linked to increased risk of cognitive decline[study]. During deep sleep at night, the brain’s glymphatic system pumps cerebrospinal fluid to clear out waste including amyloid; if sleep is poor or melatonin is suppressed, this cleaning process falters, likely accelerating plaque accumulation. Epidemiological studies show that people with sleep disorders or night shift work have higher rates of dementia. In AD patients, circadian rhythm abnormalities (like day-night confusion and sundowning agitation) are common, indicating the disease affects the brain’s clock, but it’s bidirectional circadian problems can worsen AD pathology too[Link]. Therefore, maintaining a healthy day-night cycle (“circadian hygiene”) is increasingly seen as important for prevention (more in Section 5).
Artificial electromagnetic fields (EMFs) from sources like Wi-Fi routers, cell phones (4G/5G), and other wireless devices are another modern exposure with potential impacts on brain health. While this is a contentious area with ongoing research, some animal studies suggest that low-level microwave-frequency EMFs can induce oxidative stress and even open the blood–brain barrier (BBB) under certain conditions [Link]. The BBB is a protective filtration system that prevents many toxins and inflammatory cells in the bloodstream from entering the brain. In one study, rats exposed to 900 MHz RF (a frequency used in mobile communications) for 3 hours/day over a month showed BBB leakage, neuronal edema, and degeneration in the hippocampus, along with memory deficits [Link]. The researchers found structural damage in the hippocampus and cortex of these EMF-exposed rats, suggesting that chronic exposure could make the brain more vulnerable to damage [Link]. Dr. Leif Salford’s work decades ago similarly showed that even brief cell phone radiation could allow proteins like albumin to cross the BBB in rodents, which over the long term might harm neurons [Link]. How does this relate to Alzheimer’s? If EMFs contribute to microvascular damage or BBB permeability, they could facilitate entry of unwanted substances or inflammatory molecules into the brain, exacerbating neuroinflammation a known contributor to AD. EMFs can also induce cellular stress pathways; for example, one experiment indicated activation of stress kinases (mkp-1/ERK) in the brain after EMF exposure, linked to cognitive impairment [Link]. When the blood brain barrier (BBB) is open due to exposure to high and low frequency EMF radiation substances that are not meant to enter can and substances that aren’t can leak out. This is highly problematic for the brains normal functioning and leptin/insulin regulation. I’s very wise to minimize chronic exposure to anthropogenic EMFs as recommended by anyone who understands “mitochondrial medicine,” on the grounds of the mounting evidence of harms of these man-made EMFs and of course that 3G radiation exposure tested in the 2018 National Toxicology Program (NTP) study was shown to result in cancer in nocturnal animals (less sensitive to EMF disruption than humans), and that these fields may interfere with the electrical and magnetic cues that our cells normally use. Likewise, excess blue light at night is something we can control by using blue light blocking glasses, warmer lights and screen filters. In essence, our modern lifestyle, staring at bright screens at midnight and bathing in Wi-Fi and surrounded by the AC electrical grid, imposes subtle biophysical stresses on the brain (through circadian disruption and oxidative stress) that compound over years to increase Alzheimer’s risk [Link]. Re-aligning with more natural light cycles and reducing unnecessary EMF exposure are thus considered in emerging prevention strategies (see Section 5).
Summary of Mechanistic Insights
Alzheimer’s disease is far more than just plaques and tangles. Those protein aggregates are end-stage manifestations of a breakdown in cellular homeostasis. Upstream we have: oxidative stress and redox imbalance damaging proteins; failures in mitochondrial energy production and proteostasis; disturbance of the normally structured water environment in cells; metabolic derangements like brain insulin and leptin resistance and nutrient deficiencies; and environmental stressors such as circadian rhythm disruption and anthropogenic EMF exposure. All these factors intertwine and reinforce each other: e.g., oxidative stress impairs mitochondria, which increases oxidative stress, increasing perivascular spacing, etc., in a vicious cycle. Eventually, the overwhelmed neurons accumulate misfolded proteins which themselves become toxic. By the time amyloid plaques and tau tangles are visible (whether by microscope or PET scan), the neuron’s biophysical environment has been disturbed for perhaps decades. This recognition is crucial because it means that focusing only on clearing plaques (as many past drugs have done) addresses the consequence, not the cause. Truly effective interventions will likely need to restore the cell’s healthy physics and chemistry, its redox balance, energy metabolism, and internal timing, to halt the cascade that leads to plaques and tangles. The next sections will examine how the damage to specific brain regions produces Alzheimer’s symptoms (Section 3), and then explore current and future approaches aiming to target not just the plaques, but the underlying biophysical dysfunctions (Sections 4 and 5).
Impact on Brain Regions and Manifested Symptoms
Overview
Alzheimer’s disease doesn’t hit the entire brain evenly, it starts in particular areas and then spreads, which is why certain symptoms appear early and others later. In the beginning, AD mainly damages the hippocampus and nearby regions in the brain’s temporal lobe[Link]. These areas are crucial for forming new memories and for spatial navigation (knowing where you are). That’s why short-term memory loss (like forgetting recent conversations or misplacing items) is often the first noticeable symptom. People might also become disoriented easily, even getting lost in familiar places because the brain’s internal GPS (located in the entorhinal cortex and hippocampus) is affected [Link]. As Alzheimer’s spreads to other parts of the brain, additional symptoms appear. When it reaches the parietal lobes, people have trouble with spatial skills and may bump into things or struggle with reading maps. When the frontal lobes become involved, we see changes in personality, judgment, and behavior someone might become apathetic, depressed, or occasionally agitated or paranoid. Damage to deeper and more widespread areas leads to language difficulties, inability to recognize loved ones, and loss of bodily functions in late stages. In short, the progression of AD through the brain, from memory centers outward, explains the progression of symptoms from mild memory lapses to profound dementia. This section breaks down which brain regions are most affected and how that translates into the day-to-day changes in memory, thinking, and behavior seen in Alzheimer’s patients.
The healthy brain is a finely tuned symphony of circadian-regulated processes, all interlinked through mitochondrial function, redox control, neuroendocrine signaling, and electromagnetic sensitivity. The 15 foundational systems involved, ranging from melatonin signaling, mitochondrial ATP production, glial lymphatic detoxification, POMC pathway regulation, dopamine/serotonin/acetylcholine signaling, leptin and insulin sensitivity, vagal tone, nitric oxide signaling, and redox signaling to the production of neurosteroids, neuromelanin, and biophotons, are not just parallel processes but tightly coordinated through the central clock in the suprachiasmatic nucleus (SCN) and peripheral clocks in every cell. These processes are deeply dependent on the timely presence of full-spectrum sunlight and darkness. They determine when energy should be produced, where antioxidants are needed, when the brain should detoxify, and how neurotransmitters are balanced. In Alzheimer’s disease, the breakdown of this synchronized machinery, characterized by loss of melatonin amplitude, circadian misalignment, mitochondrial dysfunction, redox collapse, and neuroinflammation, leads to impaired clearance of amyloid-β, tau tangles, insulin resistance in the brain, reduced cholinergic signaling, and loss of neuromelanin-based electromagnetic buffering. Each one of these mechanisms fails not in isolation but as part of a system-wide breakdown in bioenergetic and circadian coherence. When the timing of hormonal surges, neuropeptide production, or mitochondrial repair is off, even by a few hours, the outcome is a cumulative degradation of memory, cognition, and neural resilience.
Circadian rhythms are not optional, they are the operating system of the brain. Light and darkness are the master programmers, calibrating every single one of these 15 mechanisms daily. Morning sunlight drives cortisol and dopamine activation, synchronizes mitochondrial respiration, and programs melatonin onset 12 hours later. Evening darkness triggers sleep, autophagy, glial lymphatic detox, and synaptic pruning. However, in our modern environment, this precise system is constantly derailed. Artificial blue light at night (especially from LED lighting and screens) abolishes melatonin release and increases hippocampal and amygdalar stress reactivity. Wi-Fi and wireless devices like AirPods, acting as chronic nnEMF stressors, disrupt calcium signaling, impair mitochondrial ATP production, and elevate reactive oxygen species. Groundbreaking research by Glen Jeffery and colleagues confirms that exposure to LED light rapidly downregulates brain regions involved in memory, like the hippocampus, in animal models, while also triggering stress behavior. These findings echo what we see in Alzheimer’s: a brain operating out of sync with the light-dark cycle, flooded by toxic electromagnetic and light inputs, unable to recover, detoxify, or maintain electrochemical integrity. The solution starts not with more drugs but with restoring coherence, by entraining these 15 foundational systems through light, magnetism, hydration, and redox rhythm, aligned with nature’s original blueprint.
Targeted Brain Regions in Early Alzheimer’s
Alzheimer’s disease has a characteristic pattern of anatomical spread. The entorhinal cortex (EC) and hippocampus (located in the medial temporal lobe) are among the first regions hit by AD pathology[Link][Link]. These structures are essential for forming new memories and for spatial orientation. In fact, the entorhinal cortex is a hub that connects the hippocampus with the rest of the cortex, acting as a gateway for memory encoding. It is here that neurofibrillary tangles (tau pathology) typically begin to accumulate first, even at the mild cognitive impairment stage[Link]. The early destruction of EC and hippocampal neurons explains why short-term memory loss is the hallmark initial symptom. A person with early AD might remember events from decades ago (since those are stored widely in the cortex) but struggle to recall what they had for breakfast or the content of a recent conversation. Additionally, within the entorhinal-hippocampal circuit are specialized neurons (like grid cells) that map environments, so when these cells malfunction, spatial disorientation occurs. It’s often noted that getting lost while driving or difficulty navigating even in one’s neighborhood can appear before overt memory complaints [Link] and [Link]. In fact, research shows spatial navigation impairment can be detected in the preclinical stage of AD, sometimes even preceding measurable memory deficits [Link]. Loved ones might notice the person is more confused in unfamiliar settings or has trouble following directions.
The parahippocampal region and basal forebrain are also early targets. The basal forebrain contains the nucleus basalis of Meynert, which is the primary source of acetylcholine, a neurotransmitter important for attention and memory. In Alzheimer's disease (AD), the loss of these cholinergic neurons early on contributes to deficits in attention and memory encoding. This is why the first-line drugs for AD are cholinesterase inhibitors, which aim to boost acetylcholine levels to mitigate cognitive decline.
-
Acetylcholine: Crucial for memory encoding and attention, acetylcholine is essential for the hippocampus to form new memories. In AD, its depletion disrupts this process, leading to memory deficits and cognitive dysfunction, especially in the early stages.
Progression to Cortical Areas and Resulting Cognitive Decline
As AD advances, protein aggregates and cell death spread from the medial temporal lobe to other cortical association areas. The parietal lobes, especially the posterior cingulate and precuneus, and the angular gyrus region, are commonly affected next [Link]. These areas integrate sensory information and are involved in visuospatial processing. Damage here manifests as difficulty with visual-spatial tasks, such as trouble judging distances or placing objects in the dishwasher. This damage may also lead to anosognosia, an unawareness of their deficits, because parietal networks (especially in the right hemisphere) help us form self-appraisal of performance. The disease also affects the lateral temporal cortex, which can impair language, causing word-finding difficulty (anomia).
-
Glutamate: As the parietal lobe degenerates, glutamate dysfunction contributes to impaired spatial processing and memory retrieval. Glutamate, the primary excitatory neurotransmitter, is involved in learning and memory, and its imbalance can worsen the inability to perform complex tasks like object recognition.
By Middle Stages, Frontal Lobes Become Involved
The frontal lobes, especially the prefrontal cortex, are the executive control centers responsible for judgment, planning, problem-solving, and personality. When they are affected by AD, executive dysfunction emerges. Patients have trouble organizing tasks, following multi-step processes (like cooking a meal), or making decisions. A formerly meticulous person may become disorganized or easily distracted. Personality and mood changes often become more pronounced apathy is very common (the person loses interest in hobbies or social activities due to frontal damage). Others may experience disinhibition (saying or doing socially inappropriate things) because the frontal cortex normally suppresses such impulses (like thinking someone is stealing their belongings, when in fact they misplaced them).
-
Dopamine: The prefrontal cortex relies heavily on dopamine for executive function, and its depletion leads to difficulties with motivation and decision-making. As the frontal lobe deteriorates, dopamine dysfunction exacerbates apathy, lack of initiative, and inability to regulate emotions effectively.
-
GABA: GABA acts as an inhibitory neurotransmitter, essential for regulating impulsive behavior. Its dysregulation due to frontal cortex damage can lead to disinhibition and mood swings
Emotional Regulation: Amygdala and Limbic System
The amygdala, involved in emotion and fear, lies near the hippocampus and often accumulates pathology, contributing to anxiety or even paranoid delusions. Some AD patients develop these symptoms, like thinking someone is stealing their belongings when, in fact, they misplaced them.
-
Serotonin: Serotonin is integral to mood regulation, and its dysfunction in the amygdala can lead to anxiety and depression. As the limbic system is affected, serotonin imbalances further contribute to emotional instability, often causing agitation or apathy.
Late-Stage, Widespread Brain Involvement
In advanced Alzheimer's, damage is widespread throughout the cerebral cortex, and the brain undergoes significant atrophy (shrinkage). At this stage, global cognitive impairment is present: memory is severely impaired for both recent and distant events; language may be limited to only a few words or completely lost (aphasia); and visual recognition fails (patients may not recognize close family members or even their own reflection). This corresponds to heavy pathology in the temporal and occipital lobes, as well as the remaining cortex.
-
Acetylcholine and Glutamate: In late-stage AD, acetylcholine depletion leads to severe memory loss, while glutamate imbalances contribute to the disintegration of cognitive functions like recognition and language. These neurotransmitters are responsible for the encoding and retrieval of information; their dysfunction significantly accelerates cognitive decline.
Motor Function and Gait Impairment
The motor cortex is one of the last areas affected in AD, but eventually, coordination and motor function deteriorate, leading to difficulty walking (gait apraxia) or swallowing (dysphagia). Sensory processing can also be altered for example, some AD patients have changes in how they perceive flavors or smells (the olfactory bulbs can be impacted early in AD, which might explain why loss of smell is sometimes noted in patients years before cognitive symptoms).
-
Dopamine and Glutamate: The motor cortex, reliant on dopamine and glutamate, sees impaired function, leading to coordination difficulties. Dopamine dysfunction contributes to gait apraxia, while glutamate imbalance hampers motor learning and movement initiation.
Brain Activity and Functional Breakdown
Throughout this process, behavioral and psychological symptoms accompany the cognitive decline. In early stages, depression and anxiety are common, likely as patients sense their cognitive losses. Mid-stage can bring irritability, agitation, or repetitive behaviors, sometimes related to confusion or frustration. Late-stage often features a sort of quiet apathy; occasionally, patients develop psychotic symptoms like hallucinations or delusions.
-
Cortisol and Dopamine: Disruption of cortisol levels can lead to stress and anxiety in the early and mid-stages. In late stages, dopamine dysfunction exacerbates mood swings and apathy. Cortisol and dopamine dysregulation often leads to emotional lability and worsening symptoms.
Braak Stages of Alzheimer’s Disease
-
Stage I-II: Involve the entorhinal region, clinically silent or causing mild memory issues.
-
Stage III-IV: Spread through limbic regions like the hippocampus (mild cognitive impairment to early dementia).
-
Stage V-VI: Involve the neocortex widely (severe dementia) [Link].
To connect the biophysics to behavior: When AD destroys synapses and neurons in the hippocampus, the person cannot form new memories (because the neural circuits that encode new experiences literally disconnect or die). When neural networks in the parietal cortex break down, the person cannot integrate sensory information, leading to confusion about space and their own abilities (they might not realize they can’t do something safely). When frontal circuits are compromised, the complex orchestration of thought and action fails resulting in disorganized behavior and personality changes. Dopamine and acetylcholine dysfunction play a key role in this breakdown, impairing memory, attention, emotional regulation, and executive function. The brain operates via finely tuned electrical signals across networks; AD effectively “disconnects the wires” in a progressive manner, first in memory circuits, then spreading outward. It’s also worth noting AD tends to spare the cerebellum and primary sensory cortices until very late, so basic sensation and motor strength remain intact relatively longer, the tragedy is that patients might be physically strong but unable to coordinate or initiate meaningful action because the higher command centers are ravaged.
In summary, memory loss (especially for recent events), spatial disorientation, and mild personality changes mark the early stages stemming from medial temporal lobe damage[Link]. Worsening confusion, poor judgment, language difficulties, and mood swings emerge as the pathology spreads to parietal and frontal lobes. Inability to recognize family, communicate, or care for oneself signals extensive cortical involvement in late-stage disease. These symptoms reflect the sequential breakdown of the brain’s information-processing hubs by Alzheimer’s pathology. Understanding which brain regions are affected and when not only helps in diagnosis (for example, distinguishing AD from other dementias that might start with different symptoms), but also informs therapy e.g., memory-oriented cognitive training might help early on, whereas later care focuses more on comfort and managing behavioral disturbances.
Current Approaches to Treatment and Reversal Efforts
Overview
Treating Alzheimer’s disease is challenging because it involves a degenerative process in the brain. Mainstream medicine currently offers a few medications that can manage symptoms but don’t cure the disease. These include drugs that boost memory-related chemicals (like donepezil) or drugs that attempt to clear amyloid plaques. Recently, there’s been excitement about new antibody medications that target amyloid in the brain some have shown a slight slowing of cognitive decline in trials. However, these drugs are expensive, come with risks (like brain swelling or bleeding), and are not a magic bullet. As a result, many doctors and researchers emphasize a more holistic approach: addressing all the factors that might be contributing to the disease. This includes lifestyle changes and “whole-body” interventions. A notable example is Dr. Dale Bredesen’s protocol, which is an individualized program involving diet, exercise, sleep optimization, supplements, and more. Some patients on this program have reported improvements, suggesting that early Alzheimer’s might be reversible in certain cases if you correct the underlying issues. Additionally, emerging therapies drawing from biophysics and alternative medicine are being explored. These include things like near-infrared light therapy for the brain (shining infrared light on the head to energize neurons), using certain metabolic drugs or nutraceuticals to support mitochondria, training people to follow strict circadian routines, and dietary strategies like the ketogenic diet to fuel the brain with ketones instead of glucose. The underlying theme in these approaches is that to truly fight Alzheimer’s, we need to treat the whole person, improving their brain’s environment (light exposure, sleep, stress), their nutrition (both diet and possibly brain-specific nutrients), and their metabolic health, rather than relying solely on a single pill. Here we explore both the established treatments and these innovative strategies, from mainstream to cutting-edge, that aim not just to slow AD but potentially reverse some aspects by restoring healthy biophysical function in the brain.
Mainstream Medical Treatments
For many years, treatment for Alzheimer’s has focused on symptom management. The U.S. FDA-approved drugs for AD fall into two categories: cholinesterase inhibitors and NMDA receptor antagonists. Cholinesterase inhibitors (like Donepezil (Aricept), Rivastigmine, and Galantamine) work by preventing the breakdown of acetylcholine, a neurotransmitter important for learning and memory. By boosting acetylcholine levels, these drugs can modestly improve or stabilize cognitive symptoms in the mild-to-moderate stages of AD. Patients on these medications might have slightly better memory or ability to carry out daily tasks for a period of time[Link][Link]. The benefits are not dramatic, they do not stop the disease, but they can be meaningful (e.g., maintaining ability to converse or dress independently a bit longer). Memantine, the NMDA antagonist, is used in moderate-to-severe AD. It works on glutamate signaling to prevent excitotoxicity (overstimulation that can kill neurons). Memantine can help with cognition and behavior in later stages and is often given in combination with a cholinesterase inhibitor. These drugs address the neurotransmitter deficits caused by AD but do not affect the underlying pathology and thus fall well short of a valid solution in our books.
In recent years, a major push in mainstream research has been immunotherapy against amyloid. Monoclonal antibodies like Aducanumab, Lecanemab, and Donanemab have been designed to bind to amyloid-beta and help remove plaques from the brain. In 2021, Aducanumab became the first such drug approved (amid controversy) for AD; more recently in 2023, Lecanemab (tradename Leqembi) was approved after a clinical trial showed it could slow the rate of cognitive decline by about 27% over 18 months in early-stage patients [Link]. This means that while patients still worsened, they did so more slowly than those on placebo [Link]. This provides proof that targeting amyloid can modify disease progression, albeit modestly. Donanemab, targeting a modified form of amyloid and also showing plaque clearance, is under FDA review with similar trial results. These antibody treatments mark the first generation of “disease-modifying” drugs for AD. However, they come with caveats: many patients (about 20-40%) experience side effects called ARIA (amyloid-related imaging abnormalities), basically brain swelling or tiny hemorrhages visible on MRI [Link]. Most of these incidents are asymptomatic, but a few can be serious. These drugs also require regular infusions (e.g., every 2-4 weeks) and are extremely costly. As a result, while they are a breakthrough scientifically, they are not a simple cure and require careful patient selection and monitoring. They mainly help patients in early stages (mild cognitive impairment or mild AD) and are not indicated for moderate or late-stage AD. There are also drugs in trials targeting tau protein (e.g., anti-tau antibodies or tau aggregation inhibitors), since many believe we may need to clear tau tangles as well to see larger clinical benefits. However, these still miss the mark because they are no addressing the underlying root cause and merely chasing late stage symptoms.
Beyond pharmaceuticals, mainstream management includes addressing coexisting conditions that can worsen cognition, for example, treating B12 deficiency or thyroid disorders, controlling high blood pressure, managing diabetes, getting good sleep (treating sleep apnea if present), and managing depression or anxiety. Doctors also often recommend cognitive stimulation therapies, exercise programs, and caregiver education as part of standard care. Routine and a familiar environment are emphasized to help reduce confusion for AD patients. Essentially, while we don’t yet have a cure from mainstream medicine, a combination of available drugs and supportive measures can improve quality of life and possibly extend the time of higher functioning.
Dale Bredesen’s Multimodal “Reversal” Protocol
One of the most talked-about alternative approaches is by neurologist Dr. Dale Bredesen, who in 2014 published case reports of a comprehensive program that appeared to reverse cognitive decline in patients with early Alzheimer’s [Link]. His protocol, often called ReCODE (Reversal of Cognitive Decline) or the Bredesen Protocol, is not a single treatment but a personalized regimen addressing dozens of potential contributors to dementia. In his initial study, 10 patients with mild AD or mild cognitive impairment underwent this program, and 9 of 10 showed subjective or objective improvement within 3-6 months, some even returning to work with improved performancepu[Link] [Link]. These results were remarkable because such reversal hadn’t been documented in scientific literature before. The program’s details vary per patient but typically include: a dietary plan (often a plant-rich ketogenic or fasting-mimicking diet to enhance brain ketone usage and reduce insulin resistance), exercise (both aerobic and strength training to boost blood flow and trophic factors in the brain), sleep optimization (treating sleep apnea, practicing good sleep hygiene to ensure deep sleep for glymphatic clearance), stress reduction (meditation or yoga, since cortisol from chronic stress can worsen memory), supplements and vitamins (like omega-3 fatty acids, vitamin D, B vitamins, magnesium, tailored to correct any deficiencies), and brain training (mental exercises). It also involves more novel ideas like periodic fasting, time-restricted eating (to improve insulin sensitivity), and sometimes hormonal balance (if, say, thyroid or sex hormones are low, as they can affect cognition). The protocol targets what Bredesen identifies as various “holes in the roof” of Alzheimer’s, for example, inflammation, nutrient deficiencies, toxin exposure, and suboptimal trophic support for neurons. By plugging as many holes as possible, the brain can start to function better and even rebuild synaptic connections, according to this approach.
It’s important to note that while Bredesen’s case studies and later publications (including a 2016 paper and a 2018 report on 100 patients) are promising, they were not randomized controlled trials. Critics argue that without rigorous trials, it’s hard to know how effective the protocol truly is or which components are most important [Link]. However, many clinicians have started using Bredesen’s principles in practice (often under the term “functional medicine” for dementia). A anecdotal but compelling example: one of Bredesen’s patients, a 65-year-old woman who had to quit work due to AD, followed the program and after several months, her memory improved to the point of returning to work [Link]. These individualized successes have led to optimism that early Alzheimer’s is not necessarily a one-way street. Bredesen’s work emphasizes that Alzheimer’s has many subtypes and causes (he describes inflammatory, glycotoxic, hormonal, toxic subtypes, etc.), so a broad, personalized treatment is needed. This is very much in line with the biophysical perspective i.e., fix the underlying metabolic and oxidative issues (the “light, water, magnetism” as we’ll discuss) and the brain can heal.
Photobiomodulation (Light Therapy) and Mitochondrial Boosters
One of the emerging biophysics-based therapies for AD is photobiomodulation, which means using specific wavelengths of light to improve cellular function. In practical terms, this often involves near-infrared (NIR) light (in the range of 800–1100 nm) applied to the head or even intranasally. Why light? NIR light penetrates the skull and can be absorbed by molecules in brain cells, notably cytochrome c oxidase in the mitochondria[Link]. Absorbing these photons can stimulate the mitochondria to produce more ATP and reduce oxidative stress essentially giving an energetic jump-start to sluggish neurons[Link]. Pioneering research by Dr. Francisco González-Lima and colleagues has shown that low-level NIR laser or LED treatment can enhance brain metabolism and memory in animal models and even healthy adults[Link]. In mice engineered to have Alzheimer-like pathology, photobiomodulation led to improved cognitive performance and reduced plaque load in some studies[Link]. In humans, small studies and case reports have found that patients who undergo transcranial NIR phototherapy (for example, wearing an LED helmet or using an intranasal device at home daily) showed improvements in memory and mood. One open-label pilot on patients with dementia had them use a near-infrared light helmet (810 nm) for 6 minutes daily; after 12 weeks, they improved on cognitive assessments compared to baseline and reported better sleep and fewer angry outbursts, although a larger controlled trial is needed.
González-Lima’s work also highlights methylene blue, a metabolic enhancer, often discussed alongside NIR light[Link]. Low-dose methylene blue (an old drug) can act as an electron cycler in mitochondria, helping cells produce more energy. His experiments found that both methylene blue and NIR light, by stimulating the mitochondrial electron transport chain, can protect neurons from toxins and prevent neurodegeneration in animal models[Link]. The combined use of methylene blue (or its derivative called LMTM) with light is being explored.
On a similar note, red to near-infrared light therapy applied to the retina or eye is studied, since the retina is an extension of the brain. It’s been shown to reduce amyloid in animal models and improve retinal function, which might correlate with brain improvements, though that’s still speculative.
Another interesting light-based approach involves 40 Hz flickering light (visible light flashing at 40 times per second). MIT researchers discovered that this stimulation can entrain brain waves (gamma oscillations) and reduce amyloid and tau in mouse models, possibly by activating microglial cleanup. Early human trials with devices that provide 40 Hz light and sound stimulation daily are underway to see if it helps patients. The reason this is helpful, I speculate is because a harmonic of the Schumann resonance exists right around this level of pulse rate.
All these approaches converge on the idea of energizing the brain and reducing oxidative stress. By improving mitochondrial function, neurons might keep their circuits intact or even form new synapses. Photobiomodulation is attractive because it’s non-invasive and safe; the main question is how effective it is, which larger ongoing studies will determine. Given that neurons in AD are underpowered and emitting distress signals, giving them an energy boost with something as simple as light is a compelling strategy grounded in biophysics.
Metabolic and Dietary Interventions
As discussed, AD has features of insulin resistance in the brain, so one strategy is to alter the brain’s fuel. The ketogenic diet, which is high in fats and very low in carbs, forces the body to produce ketone bodies (like beta-hydroxybutyrate) as alternative fuels. Ketones can readily be used by brain cells and may bypass some of the metabolic block in AD brains. Clinical studies on ketogenic diets or ketone supplements in people with MCI or mild AD have shown improvements in cognitive scores while ketone levels are elevated[Link]. In a randomized trial, AD patients on a 12-week modified ketogenic diet showed significantly improved memory and cognitive performance compared to those on a regular diet[Link]. These effects sometimes diminish when patients go off the diet, suggesting it’s not curative but it boosts function while in place. The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) is another dietary approach showing epidemiological links to reduced AD risk. It emphasizes berries, leafy greens, nuts, whole grains, olive oil, and fish essentially providing antioxidants, healthy fats (omega-3s), and limiting processed foods. While not as stringent as keto, it aims to reduce inflammation and insulin resistance. Many practitioners incorporate intermittent fasting or time-restricted eating (e.g., an 8-hour eating window each day) to give the brain a metabolic rest and increase ketone periods. This can also stimulate autophagy, the cellular garbage cleanup process that might help clear protein aggregates.
Nutraceuticals and medications targeting mitochondria or oxidative stress have been tried too. For instance, coenzyme Q10, NAD+ precursors (like nicotinamide riboside), vitamin E, alpha-lipoic acid, and others are given to support mitochondrial electron transport and antioxidant capacity. Results have been mixed, but many in the mitochondrial medicine community believe a cocktail of such supplements can be supportive. There’s also interest in intranasal insulin (to overcome brain insulin resistance by delivering insulin directly to the CNS), which in some trials improved memory in MCI patients. Antidiabetic medications like metformin are being studied in non-diabetics with MCI as well, given the Type 3 diabetes angle.
Circadian and Electromagnetic Therapies
Another pillar of non-pharmacological intervention is correcting circadian rhythm disturbances. Simple measures like morning bright light exposure and evening blue-light avoidance can improve sleep quality and cognition in AD [Link]. For example, exposing AD patients to blue-enriched light during the day has been found to improve nighttime sleep and even cognitive scores modestly [Link] . This likely works by strengthening the day-night rhythm and boosting daytime alertness. Some patients are given melatonin supplements in the evening to reinforce their natural melatonin (which is often low in AD); melatonin not only aids sleep but is neuroprotective. Physical activity during the day also reinforces circadian cues and has the benefit of increasing BDNF (a growth factor important for neuron survival). On the flip side, minimizing exposure to possibly harmful EMFs by turning off Wi-Fi at night, keeping cell phones away from the head (using speaker or text instead), and avoiding living near high-voltage power lines, is an obvious strategy to employ to protect the brain and allow it to heal. The idea is to reduce any source of oxidative stress or BBB disruption that could be burdening the brain. Additionally, some advocate grounding or earthing (making skin contact with the earth or if not in the presence of live power using a grounding sheet/mats) to tap into the earth’s electrons and potentially stabilize the body’s electrical environment aligns with the “magnetism” aspect of health that aids in lowering chronic inflammation, one of the hallmarks of Alzheimer’s.
Rehabilitation and Cognitive Training
Cognitive stimulation, memory exercises, and brain training programs are wise to incorporate into managing AD; not using technology screens, instead real-life situations or physical props. Social engagement and learning new skills (within the person’s capacity) also stimulate the brain and can be incorporated. Something like learning to dance or doing art therapy combines physical, cognitive, and social stimulation, a holistic approach that has shown positive effects on mood and cognition.
Putting It All Together: Multidomain Lifestyle Trials
The growing understanding that Alzheimer’s disease (AD) has multifactorial origins has sparked groundbreaking trials testing combined lifestyle interventions. A prime example is the Finnish FINGER trial, which demonstrated that a holistic approach, including diet, exercise, cognitive training, and vascular risk management, led to measurable cognitive improvements in at-risk older adults over just two years. This groundbreaking work is part of a wave of international studies (such as U.S. POINTER) that are exploring whether targeting multiple lifestyle factors simultaneously can significantly slow or even prevent cognitive decline. Early results are already showing great promise, participants on these programs not only preserve cognition better, but even those already diagnosed with AD show improvements in quality of life and slower disease progression.
Genetics like APOE4 status do play a role, carrying the APOE4 allele raises risk of AD – but even APOE4 carriers are now shown to benefit greatly from lifestyle interventions. For instance, APOE4-positive individuals on a ketogenic diet or intensive lifestyle program can sometimes normalize their cognitive function, showing that genes are not destiny. In fact, many see APOE4 as a genotype that makes one more sensitive to environmental and lifestyle factors (like diet and sleep), meaning those factors become even more crucial to manage.
But this is just the beginning. As research advances, we are beginning to understand the profound influence of light on mitochondrial function in AD. Emerging therapies, such as heliotherapy, photobiomodulation, grounding, and the mitigation of artificial narrow-band blue light and anthropogenic electromagnetic fields (EMF), hold the potential to prevent and reverse AD in ways that current pharmaceuticals or cognitive training tools could never achieve. The paradigm is shifting, no longer must we accept the notion that our genes alone determine our health trajectory. By delving into the biophysics of light, both visible and non-visible, and understanding its intricate effects on the brain through melanin, water, circadian rhythms, neurotransmitters, and mitochondria, we are paving the way toward an end to Alzheimer’s. The future is bright, and it’s in our hands to rewrite the story of how we protect and enhance brain health.
What all these approaches underscore is that real healing in Alzheimer’s likely requires addressing the root causesm, oxidative stress, inflammation, insulin and leptin resistance, toxin exposure, nutrient deficiencies, lack of neurotrophic support, rather than just the end result of amyloid plaques. In Bredesen’s words, just removing plaques while the “roof is full of holes” (ongoing insults) is not sufficient. This is why he and others emphasize focusing on fundamental factors often phrased as “light, water, and magnetism”, essentially meaning: correct the light environment (circadian rhythm and beneficial light therapies), optimize the water and biochemistry inside the body (hydration, nutrition, redox state, deuterium levels), and address magnetism (natural electromagnetic balance and minimizing artificial EMF stressors).
In summary, while mainstream medicine in 2025 can offer symptomatic relief and the first glimmers of disease-slowing via anti-amyloid drugs, a truly effective treatment or reversal of Alzheimer’s is more likely to come from a multi-pronged strategy. Combining medications (old and new) with lifestyle optimization and possibly novel therapies (light, metabolic drugs) is an approach already being practiced in some clinics. We are moving away from the idea of a single silver-bullet pill and toward treating AD like the complex systemic disease it is. The next section will look ahead to what the future might hold if these biophysics-informed strategies become more mainstream – potentially transforming AD from a feared irreversible decline into a manageable, even preventable condition.
Future Perspectives: Prevention and Treatment through a Biophysical Lens
Overview
Looking to the future, there is a hopeful vision: Alzheimer’s disease could become a preventable and even reversible condition. The path to that future isn’t a single wonder drug, but rather a better understanding of how our everyday life affects our brain health. We’re learning that by the time someone has memory loss, the disease has been quietly building for 20 years. So the future of fighting AD is all about early detection and early intervention. This might mean in your 40s or 50s you get a simple eye scan or blood test that tells you your brain is starting to collect abnormal proteins, and then you immediately start a prevention program. That prevention would likely focus on personal responsibility: optimizing your sleep habits, diet, exercise, and environment (light exposure, reducing chronic stress, etc.). Think of it as maintaining “brain hygiene” throughout life, much like we maintain dental hygiene to prevent cavities. Advancements in technology like Retinal OCT scans and hyperspectral imaging (scans of the retina at the back of your eye) are showing promise to detect Alzheimer’s changes years before symptoms, since the eye can act as a window to brain health. In the future, a quick, non-invasive retina scan might flag at-risk individuals who can then act long before any memory loss begins. Or if you want to take the precautionary approach like many health-conscious individuals and want to prevent all brain diseases you can aim to improve your lifestyle choices daily and not need to undergo any diagnostic testing because you already know your doing what you need to do to prevent brain disease.
The future of Alzheimer’s prevention will be in our kitchens, our bedrooms (where we set our sleep schedule), and our daily routines, not just in the pharmacy. By embracing this biophysics-informed lens, viewing Alzheimer’s as a breakdown of the body’s natural balance with light, water, and electromagnetism, future strategies will likely integrate ancient wisdom (sunlight, rhythm, nutrition) with cutting-edge science (gene editing, stem cells, advanced imaging). Personal responsibility and lifestyle optimization will be central, because no pill can substitute for a healthy environment for our neurons. Let’s explore these future directions in a bit more detail.
Early Detection and “Know Your Brain” Culture
One of the most promising developments is the push toward early detection of Alzheimer’s changes, before irreversible damage is done. Currently, definitive diagnosis often relies on PET scans or spinal taps for amyloid and tau, which are expensive or invasive. Future screening might be far simpler. For instance, the retina in our eyes has been found to show AD-related changes, thinning of certain layers, changes in blood vessel density, and even deposits of amyloid protein. Modern imaging like OCT (Optical Coherence Tomography) can measure retinal layers with microscopic precision, and OCTA (OCT Angiography) can assess retinal blood flow. Studies have shown that patients with early AD or even mild cognitive impairment have a thinner retinal nerve fiber layer and other retinal irregularities compared to healthy peers [Link]. These retinal changes correlate with brain atrophy and plaque load [Link] and [Link]. In the near future, it’s likely that routine eye exams for older adults will include OCT scans; if your retina is thinning faster than normal, it could prompt a closer evaluation of your brain health. Additionally, hyperspectral imaging, which analyses the way light of different wavelengths is reflected by the retina, can detect subtle changes in tissue composition. A new imaging device combining OCT with light-scattering analysis was able to detect that the retinal layer in AD models is not only thinner but also “rougher and more disordered,” indicating structural changes due to disease [Link]. This kind of photonic fingerprint of AD could serve as an early biomarker. In fact, researchers at Duke engineered a prototype that measures retina thickness and texture; it could potentially become an easy screening tool at clinics and even pharmacies {Link] and [Link]. The idea is a person could get a quick, noninvasive retina scan in middle age that tells them their risk status.
Similarly, we may see blood tests that measure specific protein fragments or inflammatory markers that signify Alzheimer’s changes. Although these are likely not likely ideal for early detection they can be paired with retinal OCTs and Hyperspectral Pigment Imaging or magnetic encephalogram (MEG) scans. Blood tests for amyloid and phosphorylated tau are in development and showing high accuracy in research. Coupled with genetic information (like APOE status), one might get a “dementia risk score” before we are currently diagnosing them at present, to identify any cognitive issue. The challenge then will be: what do you do with that information? This is where a culture shift is expected, a shift to lifestyle and environmental medicine practices becoming the norm. A high-risk individual might work with a coach or physician to implement a comprehensive prevention plan.
Preventive Lifestyle as Mainstream Medicine
In the future, when someone is identified at risk for AD (through those tests or due to family history), the first prescription might be lifestyle changes rather than pharmaceuticals. We might have “Brain Health Programs” covered by insurance that include consultations with biophysicists, building biologists, nutritionists, exercise physiologists, and sleep specialists, all geared to optimize those pillars of brain wellness. For example, a person might be “prescribed” a Building Biology (including artificial light and EMF mitigation) assessment of their home, a small package of blue light blocking glasses, faraday bag for their phone, red/infrared light device and a 12-month program of diet, exercise, cognitive training and stress reduction and then be re-evaluated. This is already happening in some forward-thinking memory clinics, but it will become routine. The earlier it starts, the better – even in one’s 30s and 40s, following general brain-healthy habits likely pays off decades later (given AD pathology often starts in the 50s or 60s).
Technological Aids will also assist personal responsibility. We might wear devices that allow airplane mode to remind us to get bright full spectrum natural light in the morning or to dim lights at night, or alarms that tell you when to put on your blue light blocking glasses and switch the warm indoor lights on in the evening. As well as smart Wi-Fi routers that turn off when not in use or phones that automatically pulse less radiation when not in use. Low EMF sleep trackers can detect if we’re not getting enough deep sleep (when amyloid is cleared) and prompt interventions. Diet apps could help ensure we get enough omega-3s and not too many refined carbs each day. In short, biofeedback and smart tech might make it easier to adhere to a brain-healthy lifestyle by personalizing advice and monitoring our success.
Evolution of Medical Therapies
On the medical front, current anti-amyloid drugs are just the beginning. We anticipate combination therapies will be investigated, for instance, combining an anti-amyloid antibody with an anti-tau treatment and an anti-inflammatory agent. There’s recognition that hitting multiple targets (like the multi-pronged lifestyle approach) pharmacologically might be necessary. Future drugs might include mitochondrial protectors (some are being studied, like compounds that activate PGC-1α, the master regulator of mitochondrial biogenesis, or drugs that enhance mitophagy to clear out defective mitochondria), and neurotrophic factors (like BDNF mimetics to help neurons form new synapses).
One exciting area is regenerative medicine: for instance, using stem cells or exosomes to repair brain tissue. While the adult brain doesn’t regrow large areas, there’s evidence that stem cell infusions or certain growth factor infusions can promote neurogenesis in the hippocampus and improve function. Trials are ongoing to see if injecting cells or exosomes (which are like little packets released by stem cells containing growth signals) can slow cognitive decline.
However, even as these therapies develop, they will likely work best in an environment where the brain is not constantly bombarded by preventable stressors. For example, a tau-clearing drug might remove tangles, but if the person continues to have uncontrolled diabetes and severe sleep apnea, the tangles might just reform. Thus, even future drugs will likely be adjuvants to lifestyle.
Integration of Biophysics in Daily Life
The future could see some interesting integrations of biophysical concepts: home devices for photobiomodulation (maybe a “smart lamp” that emits NIR light during your evening relaxation to help your neurons recover from the day), saunas or hyperthermia therapy (to induce heat-shock proteins that help refold misfolded proteins), and cold therapy (cold showers or cryotherapy, which can also stimulate beneficial stress responses and reduce inflammation). These “biohacks,” currently popular in certain wellness circles, might gain evidence and become part of preventive regimens. They all revolve around triggering the body’s natural repair mechanisms (hormesis).
Moreover, an appreciation of natural environments may re-emerge as therapy. There is research that spending time in nature, with exposure to natural light and grounding and an absence of urban noise/EMF, can reduce stress and potentially benefit circadian alignment. We might see “brain health retreats” where people go for a week to reset their rhythms ,waking with the sun, doing physical activity, eating farm-to-table food, avoiding digital devices at night, etc. basically a retreat to practice an ideal routine that one can then try to implement at home.
Empowered Patients and Society
Perhaps one of the biggest shifts will be in societal approach. Just as awareness campaigns taught people about heart-healthy lifestyles or how to prevent cancer (sun protection, not smoking, etc.), we’ll have brain health campaigns. People will know terms like “cognitive reserve” (the idea that education and mental engagement build a reserve that delays dementia onset) and will be encouraged to pursue lifelong learning, social engagement, and creative hobbies to build that reserve. The stigma of dementia may lessen as we talk about it more openly and focus on prevention and early action. Communities might organize programs for older adults to engage in exercise and cognitive games together, blending social and cognitive stimulation (some communities already have “dementia-friendly” initiatives, which will expand).
Personal Responsibility: A Double-Edged Sword
The emphasis on personal responsibility has great potential but also must be handled with care. Not everyone has equal access to healthy foods, safe places to exercise, or medical guidance. The future ideal would involve making brain-healthy living accessible to all, for example, urban planning that ensures anthropogenic EMF radiation-free zones with green spaces and safe walking areas for exercise, regulations that encourage healthier food options and discourage junk food, initiatives to reduce air pollution (since air pollution particles have been found in brains and may contribute to AD), and possibly providing financial incentives or support for those engaging in prevention programs (much like insurers now might lower premiums if you don’t smoke or if you go to the gym regularly). Suburbs where streetlights dim to warm orange light after 9pm and lighting in hospital/schools/nursing homes and malls that are required to be full spectrum circadian (including infrared) that change throughout the day mimicking the solar spectrum (without significant levels of ultraviolet) in that location. The healthcare system may need to adapt to spend more on prevention up front, which pays off in fewer dementia cases decades later.
Personal responsibility also means each of us educating ourselves and taking action, rather than assuming “there’s nothing I can do; I’ll just get a pill when it happens.” As more success stories emerge from people improving through lifestyle, it will motivate others. The message is that stacking the odds in your favor is possible and worthwhile. Even if one is genetically predisposed (say, APOE4 positive), embracing a biophysically sound lifestyle could mean the disease never actually manifests in one’s lifetime, effectively compressing morbidity to the very end of life or dodging it entirely.
The Role of Society and Technology in Magnetism
One interesting future angle is addressing the “magnetism” part of “light, water, magnetism.” This could involve re-examining how we design technology and infrastructure to be biologically friendly. For instance, engineers might develop Wi-Fi or telecommunications technologies with frequencies and modulation schemes that minimize biological interference. And as building biology becomes more popular it may be subsidized by governments or adopted by private companies as a competitive advantage such as ‘Biospectral Healthy Homes Certification’. There will be more research done on exposure of multiple high-powered devices at once on children so the radiation exposure guidelines can be changed and industry are forced to become better at designing safer technology. The key is that we’ll align our technology with our biology rather than ignore biology. Similarly, indoor lighting standards might change, more circadian lighting in workplaces and elder care facilities (bright blue-rich light in daytime, dimmer warm light in evenings) to support healthy rhythms, which can impact dementia outcomes.
In essence, the future ideal scenario is preventative maintenance of the brain throughout life, using early detection tools and broad-based lifestyle modifications as the first line of defense. Medications and high-tech treatments will play a supportive role, especially for those who still develop symptoms. The concept of “curing” Alzheimer’s may transform into “managing Alzheimer’s” much like a chronic condition, with many individuals never progressing to severe stages because of combined interventions. We might see the average age of onset pushed later and later – perhaps many people will live into their 90s cognitively intact, where in the past they might have gotten AD in their 70s.Currently the average age of diagnosis is 72 as at 2025, down from 74 in 2020, and it’s set for a reduction in 2030 to 70, let’s stop this and turn it back the other way!
The biophysics health perspective encourages people to get early morning full spectrum light exposure, drink clean deuterium depleted water, avoid excessive artificial stimuli, and keep their redox state healthy, essentially to live in harmony with our biology. This does not just potentially prevent AD, but enhances quality of life (better sleep, better mood, more energy). So, the drive toward Alzheimer’s prevention could have the side benefit of making society healthier overall.
By marrying high-tech advances (like retinal imaging and precision medicine) with foundational health wisdom (like waking/sleeping with the solar cycle, eating real food, and staying active), we stand on the brink of transforming Alzheimer’s from an unstoppable degenerative disorder into a manageable condition or something one can sidestep entirely. The personal and societal commitment to brain-healthy living, begun early and sustained diligently, is poised to become the cornerstone of ending the Alzheimer’s epidemic.
Retina Scans: A Glimpse of the Future Now, It’s worth noting as a concrete example: Retinal OCT and hyperspectral imaging techniques are already in trial use to detect AD. These methods leverage the fact that the retina filters and reflects light differently once neurodegeneration sets in. Changes like a patchy thinning of the retinal nerve fiber layer or altered light reflection could alert doctors of “Alzheimer’s in the making” [Link] and [Link]. In the future, an ophthalmologist could be one of your first Alzheimer’s preventers, spotting microscopic changes in an eye scan and teaming up with a neurologist or decentralized lifestyle/environmental medicine specialist to get you on a prevention plan. This synergy of diagnostic technology and preventative therapeutics exemplifies how a biophysical approach (optical imaging) combined with lifestyle medicine could dramatically alter outcomes.

To sum up, the emerging consensus for the future is: Alzheimer’s disease is multifactorial and thus demands multifactorial solutions. We will treat the person, not just the plaques. Everyone – from individuals making daily choices to healthcare providers and policy makers, will have a role in this paradigm. Education will be key: people need to know that what’s good for the heart is also good for the brain, and additionally, that things like consistent sleep, life-long learning, and managing stress are not just feel-good advice but potentially lifesaving actions for the brain. With broad adoption of these principles, we could see significantly fewer cases of Alzheimer’s in coming generations. And for those who still develop it, their journey might be milder and slower, supported by a range of therapies that keep them connected to their loved ones and world far longer than is currently possible. It’s an inspiring vision, one where Alzheimer’s is no longer a dreaded, helpless fate but a challenge that can be met proactively with science-backed measures. The groundwork is being laid now, and the coming years will test and refine these strategies, hopefully ushering in an era where “Alzheimer’s prevention” is as commonplace.
References
-
Bredesen, D. E. (2014). Reversal of cognitive decline: A novel therapeutic program. Aging (Albany NY), 6(9), 707–717pubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov.
-
Gonzalez-Lima, F., & Auchter, A. (2015). Protection against neurodegeneration with low-dose methylene blue and near-infrared light. Frontiers in Cellular Neuroscience, 9, 179[Link]. doi:10.3389/fncel.2015.00179
-
GBD 2019 Dementia Forecasting Collaborators. (2022). Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. The Lancet Public Health, 7(2), e105–e125[Link]. doi:10.1016/S2468-2667(21)00249-8
-
Jucker, M., & Walker, L. C. (2013). Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature, 501(7465), 45–51. doi:10.1038/nature12481
-
Maurer, K., Volk, S., & Gerbaldo, H. (1997). Auguste D and Alzheimer’s disease. The Lancet, 349(9064), 1546–1549. doi:10.1016/S0140-6736(96)10203-8
-
Nguyen, T. T., et al. (2020). Type 3 diabetes and its implications in Alzheimer’s disease. Biomedical Journal, 43(4), 428–441[Link][Link]. doi:10.1016/j.bj.2020.07.007
-
Phillips, M. C. L., et al. (2021). Randomized crossover trial of a modified ketogenic diet in Alzheimer’s disease. Alzheimer’s Research & Therapy, 13(1), 51. doi:10.1186/s13195-021-00783-x
-
Tang, J., et al. (2015). Exposure to 900 MHz electromagnetic fields activates the mkp-1/ERK pathway and causes blood–brain barrier damage and cognitive impairment in rats. Brain Research, 1601, 92–101mdsafetech.org. doi:10.1016/j.brainres.2015.01.019
-
Retinal Biomarkers in AD: Zhang, Y., et al. (2021). Advances in retina imaging as potential biomarkers for early diagnosis of Alzheimer’s disease. Translational Neurodegeneration, 10(1), 6translationalneurodegeneration.biomedcentral.com translationalneurodegeneration.biomedcentral.com. doi:10.1186/s40035-021-00230-9
-
Livingston, G. et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet, 396(10248), 413–446[Link] link.springer.com. doi:10.1016/S0140-6736(20)30367-6

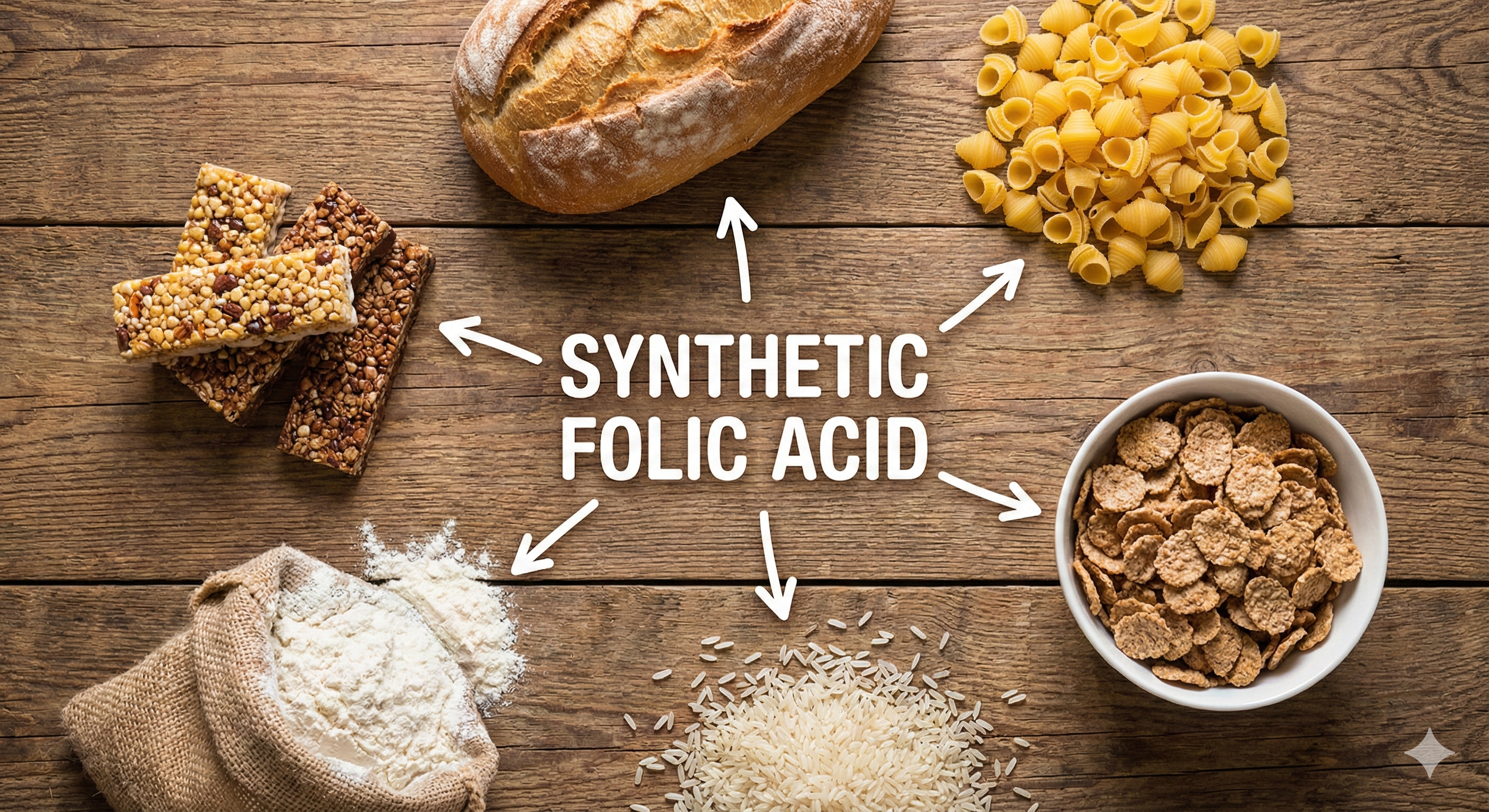

Disclaimer
The information on this site is provided by BioSpectral Systems for educational and informational purposes only. It is not intended to diagnose, treat, cure, or prevent any disease and has not been evaluated by the U.S. Food and Drug Administration or any other regulatory authority. Always consult a qualified healthcare professional before making any changes to your health regimen. By using this site, you acknowledge that you do so at your own discretion and agree that BioSpectral Systems, its affiliates, and contributors are not liable for any outcome resulting from the use of the information presented.
Share:
What is Leptin?? Only the Most Important Hormone to Human Health!
Do Blue Light Glasses Work? Why Your Clear Blue Light Glasses May Be Doing Nothing