What is GLP-1, really?
GLP-1 stands for Glucagon-Like Peptide-1, a hormone released from your gut when you eat. But it’s more than just a satiety switch, it links your light exposure, food timing, and circadian rhythm to your metabolism and brain performance.
What does GLP-1 actually do?
-
Tells your brain: “You’re full, we’re safe.”
-
Slows down digestion
-
Regulates blood sugar
-
Improves insulin sensitivity
-
Reduces chronic inflammation
-
Helps burn fat when functioning well
-
Protects your heart and arteries
-
Shields the brain from degeneration (yes, including Alzheimer’s)
Why does everyone keep talking about it?
Because it’s the key hormone that Ozempic and Wegovy mimic, but your body makes it naturally. Pharmaceutical versions work, but they hijack a natural feedback loop that was designed to work with light, food, and movement.
Here’s the real story behind the hype
Celebrities promote GLP-1 drugs like a miracle fix, but those injections can’t fix broken light environments, late-night eating, or chronic stress. These drugs mimic biology, but they don’t restore it. Real healing comes from recalibration, not substitution.
Is it too good to be true?
Yes, if you think an injection will replace healthy choices.
No, if you realize you can reawaken GLP-1 naturally by aligning with nature.
There is no miracle drug, but there is a miracle design. You’re living in it.
What shuts down your GLP-1 system?
-
Eating late at night
-
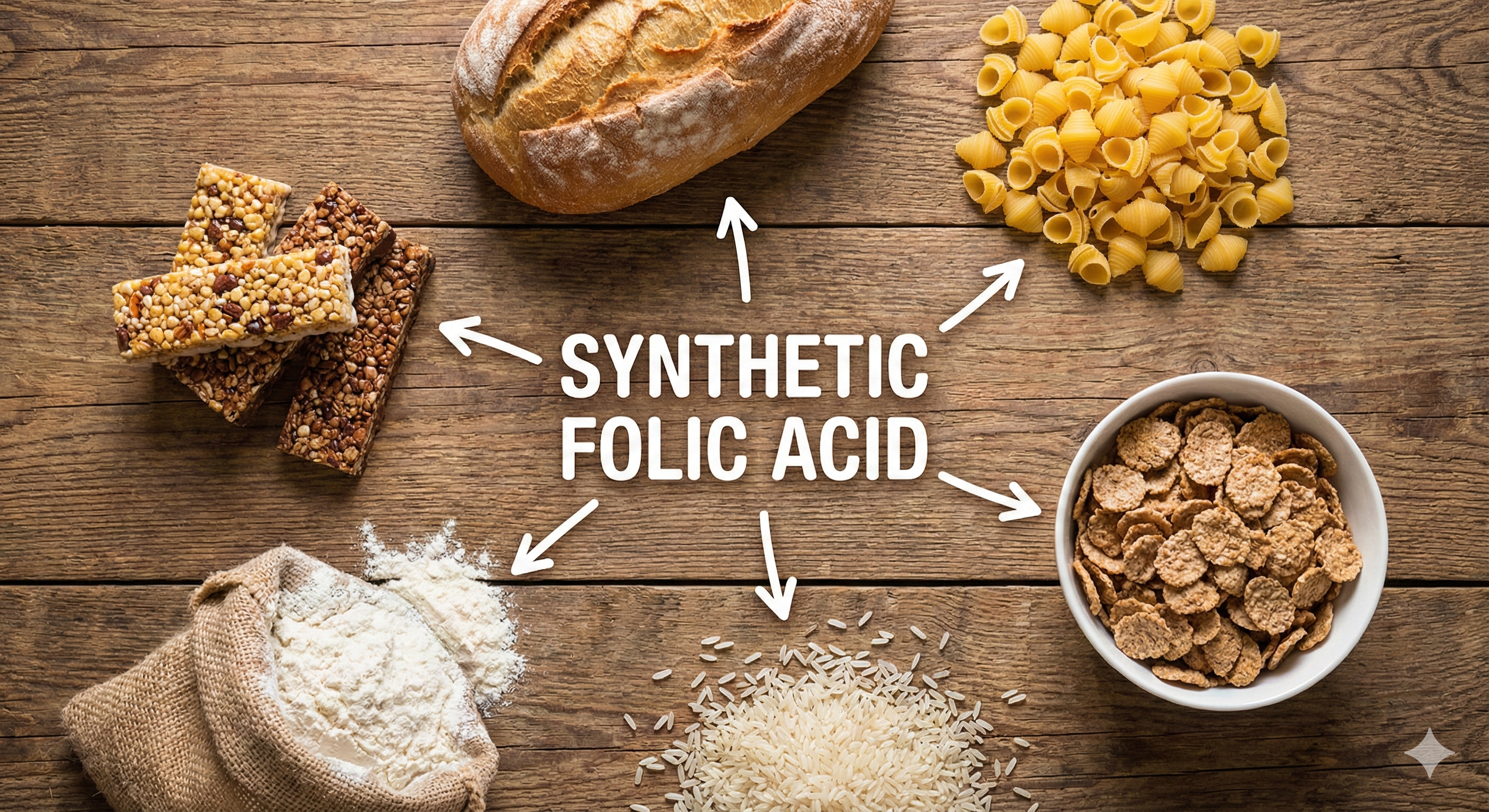
Ultra-processed foods
-
Seed oils, refined sugar
-
Artificial light after sunset
-
Inconsistent sleep
-
Chronic stress and cortisol overload
-
Poor gut health
The good news: You don’t need a drug.
Your body knows how to activate GLP-1. With the right signals, from food, movement, sunlight, and timing, you can turn it back on without side effects.
How to boost GLP-1 naturally
-
Morning sunlight (infrared + UVA triggers the gut-brain axis)
-
High-protein meals, especially at breakfast
-
Fiber-rich vegetables and fermented foods
-
Healthy fats like eggs, wild salmon, ghee, olive oil
-
Polyphenols (berries, green tea, cacao)
-
Circadian-aligned eating: no late-night snacking
-
Movement, especially after meals
-
Grounding and nervous system regulation
-
7–9 hours of quality, dark, cold sleep
Why GLP-1 actually matters
Because hunger, metabolism, energy, brain function, and even longevity depend on it. GLP-1 doesn’t just help you feel full, it helps you feel aligned, capable, and clear. And when it flows, your body expresses energy as movement, healing, thought, and creativity, not inflammation or confusion.
Introduction to GLP-1 and Its Role in Metabolic Regulation
Glucagon-like peptide-1 (GLP-1) is a hormone naturally produced in the intestines in response to a diverse range of stimuli, including food intake, light exposure, water intake, microbiome diversity, exercise, and thermal or cold stress. It plays a critical role in regulating insulin secretion, controlling blood glucose levels, and slowing gastric emptying. Endogenously, GLP-1 is secreted by the L-cells of the small intestine as part of the proglucagon peptide, which is cleaved into its active form by enzymes such as prohormone convertase 1/3.
While food intake is a key driver of GLP-1 secretion, its production is also significantly influenced by circadian light/dark cycles (which regulate enteroendocrine function through light-dependent mitochondrial activity), hydration status (via gut stretch receptors and osmolarity changes), microbiome signaling (including bacterial light, gas, and electrical signals), exercise (which promotes enteroendocrine activity through mechanical and metabolic pathways) and cold exposure (which activates brown adipose tissue and gut-hormone signaling). This broad sensitivity to environmental and physiological signals allows GLP-1 to function as a metabolic integrator, aligning energy regulation with the body's internal and external conditions to maintain homeostasis and adapt to varying demands.
GLP-1 Drugs: Synthetic Amplification Drawbacks
GLP-1 receptor agonists, such as Ozempic, are synthetic versions of this hormone designed to override/amplify its natural processes. These drugs increase insulin secretion in response to elevated glucose levels, suppress glucagon, slow gastric emptying, and signal the brain to reduce appetite. This has positioned them as attractive solutions for managing Type 2 diabetes (T2D) and promoting weight loss. However, their action is limited to attempting to mimic food-induced GLP-1 activity and does not account for the hormone’s responses to other stimuli such as light, water, or thermal stress, leaving broader metabolic processes unaddressed, which underline all modern human chronic disease states. For instance, GLP-1’s role in circadian synchronization and mitochondrial health, critical for optimal hormone balance and leptin signaling, remains unresolved by synthetic agonists. While these drugs attempt to provide short-term metabolic control, they fail to target root causes of metabolic dysfunction present like mitochondrial dysfunction (impaired signaling and energy/water production), hormone dysregulation (leptin resistance and melatonin deficiency), and impaired cellular adaptive flexibility.
GLP-1 signals satiety to the brain through an intricate mechanism involving neural pathways, vagal communication, and regulation of reward centers. Upon release from the intestines in response to food and non-food stimuli (such as cold exposure or hydration), GLP-1 activates receptors in the hypothalamus, particularly in the arcuate nucleus (ARC) and paraventricular nucleus (PVN). These regions regulate appetite by suppressing hunger-promoting neurons (AgRP/NPY) and stimulating appetite-suppressing neurons (POMC/CART) within the leptin-melanocortin pathway. GLP-1 also interacts with the vagus nerve, transmitting satiety signals from the gut to the brainstem’s nucleus tractus solitarius (NTS), enhancing satiety responses. Additionally, it influences the brain’s reward centers, such as the ventral tegmental area (VTA), modulating dopamine release and reducing food-seeking behaviors. These mechanisms allow GLP-1 to integrate diverse metabolic, hormonal, and neural signals, ensuring precise energy regulation. However, synthetic GLP-1 drugs primarily target food-triggered pathways, artificially increasing insulin secretion, overlooking the hormone’s broader role as a responder to environmental cues and physiological states.
How is Insulin supposed to be regulated? Insulin is a Circadian Hormone designed to be yoked to light/dark cycles. Insulin regulation is tightly synchronized with the circadian rhythm, which is governed by light exposure through the eyes, skin and gut. This light activates melanopsin in the retina and subcutaneous fat, signaling the suprachiasmatic nucleus (SCN) to align insulin secretion with daytime activities like eating and energy expenditure while suppressing it at night to prioritize cellular repair. GLP-1, naturally integrated into this circadian system, adjusts its secretion to metabolic and environmental demands. Synthetic GLP-1 drugs, however, artificially manipulate insulin rhythms, decoupling them from the circadian and intracellular clocks that regulate organ function. This creates stress on the pancreas, gastrointestinal tract, kidneys, and gallbladder, driving further metabolic and hormonal imbalances and opening risks in these organs as evidenced in emerging research. The positive and negative feedback loops which connect all endocrine secretions across the human living system are intertwined who’s diverse functions are much more complex than just one input and one output, there are collateral impact of every biochemical decision made. Just like turning on and off certain genes results in multiple outcomes beyond the one desired, as does the adaptive epigenome when targeted via a very specific drug, such as a GLP-1 agonist. Failing to synchronize with the natural feedback loops of leptin, melatonin, and cortisol, these drugs disrupt the intricate harmony required for sustained metabolic health.
Short-Term Benefits, Long-Term Risks
GLP-1 receptor agonists offer notable short-term benefits, such as weight loss and improved blood sugar control, but their limitations make them far from a comprehensive solution. These drugs are not a cure for diabetes or obesity but merely a management tool that suppresses appetite and slows gastric emptying, without addressing the underlying metabolic dysfunction. By masking the hallmarks of metabolic disease such as mitochondrial dysfunction, leptin resistance, and hormonal imbalances, they act as a "band-aid" solution, offering temporary fixes while leaving root cause health risks unaddressed.
While these drugs suppress appetite and enhance glucose control, they interfere with GLP-1’s natural adaptability to diverse environmental and physiological stimuli, especially light and darkness signals and the subsequent myriad of cascading biochemical reactions. This diminished adaptability results in reduced stress tolerance across all domains, whether environmental, emotional, psychological, or physical. Over time, the overstimulation of GLP-1 receptors disrupts metabolic flexibility, impairing the body’s ability to adapt to fluctuating conditions and compounding its vulnerability to chronic diseases.
Prolonged use of synthetic GLP-1 agonists exacerbates this dysfunction by increasing the risk of side effects like nausea, pancreatitis, and gallbladder dysfunction. These drugs also disrupt hormonal balance and energy regulation, impairing the body’s physiological responses to stress. This weakened stress tolerance extends to neurotransmitter and hormonal systems, often leading to poor decision-making, mood instability, and behavioral disruptions, which is beginning to show up in anecdotal feedback from GLP-1 drug users. Such destabilization is indicative of deeper systemic issues, including impaired mitochondrial signaling and misaligned circadian, ultradian, and infradian rhythms, processes that regulate everything from sleep/wake cycles and digestion to appetite and reproductive health.
The psychological impact of these drugs is equally concerning. By interfering with critical hormone rhythms like insulin, leptin, melatonin, and cortisol, synthetic GLP-1 agonists contribute to destabilized mood and behavioral health. This disruption raises serious questions about the long-term effects of decoupling these finely tuned hormonal pathways, which are intricately tied to overall metabolic and emotional well-being.
The weight loss achieved with GLP-1 receptor agonists is primarily driven by appetite suppression and delayed gastric emptying, creating a prolonged sense of fullness. While this mechanism can be appealing for those struggling with overeating or food cravings, it fails to address the root causes of weight gain, such as mitochondrial dysfunction, leptin resistance, and disrupted circadian alignment. The weight loss achieved is often temporary and dependent on continued use of the medication. Once the drug is discontinued, many patients experience weight regain, highlighting the transient nature of this approach.
Ultimately, synthetic GLP-1 agonists disrupt more than they solve. They reduce metabolic flexibility, impair the body’s natural ability to respond to environmental and dietary changes, and fail to address the foundational issues driving chronic metabolic diseases. By prioritizing short-term benefits at the expense of long-term health, these drugs leave patients trapped in a cycle of dependency, with new risks compounding existing dysfunctions.
Why GLP-1 Drugs Fail to Address the Real Problem
GLP-1 drugs, such as Ozempic, are often praised for their ability to lower blood glucose levels and promote weight loss. However, these drugs focus solely on managing the symptoms of metabolic disease, leaving the underlying causes, leptin resistance, mitochondrial dysfunction, and hormonal dysregulation, unaddressed. This oversight perpetuates the cycle of chronic illness, contributing to conditions such as Type 2 diabetes, obesity, metabolic syndrome, Alzheimer’s disease, and autoimmune disorders. By ignoring these root dysfunctions, GLP-1 drugs fail to halt the progression of the metabolic crises affecting millions today.
Mitochondria, the powerhouses of the cell, are central to human health. They produce ATP (the body’s energy currency), synthesize hormones, create hemoglobin and signaling peptides, generate intracellular water, and release carbon dioxide, the critical driver of every breath. In individuals with metabolic dysfunction, mitochondrial efficiency plummets, leading to inadequate energy production and an over-reliance on glucose for fuel. This inefficiency drives the insulin resistance, leptin resistance, and chronic inflammation that form the foundation of metabolic disease.

When mitochondrial function is compromised, the body’s intricate signaling systems break down. A state of metabolic imbalance emerges, leaving the body unable to perform essential functions. It cannot accurately regulate hunger, thirst, or sleep, detoxify effectively, sustain energy for physical activity, or adapt to natural full-spectrum light without triggering a photophobic reaction. This disruption extends to immune function, hormonal balance, and even the body’s capacity to repair itself, amplifying susceptibility to chronic illnesses and emotional instability.
GLP-1 receptor agonists exacerbate these issues by targeting a single pathway, insulin regulation, while neglecting the broader context of metabolic dysfunction. The result is a cascade of biochemical chaos, with increased inflammation, oxidative stress, and further impairment of mitochondrial signaling. These downstream effects manifest as psychological, emotional, and physical disruptions, as evidenced by blood test abnormalities and adverse reactions reported by users.
This myopic approach is akin to patching one cog in a complex machine while ignoring the larger interconnected system. For individuals living with chronic metabolic diseases, whether it’s pre-diabetes, obesity, or chronic fatigue syndrome, this fragmented intervention only deepens the body’s dysregulation. The temporary benefits offered by GLP-1 drugs come at the cost of long-term metabolic adaptability and resilience, leaving the body more vulnerable to its original dysfunctions and the burden of new side effects.
What’s the real problem?
Insulin is not the master hormone, Leptin is:
Leptin, often referred to as the “master hormone,” plays a pivotal role in regulating growth, energy balance, and metabolic health. It acts as a vital communicator between brain mitochondria and body mitochondria, signaling when energy stores are sufficient. This signal suppresses hunger and promotes fat burning during sleep, helping the body maintain energy balance. Proper leptin regulation allows for adaptation to seasonal changes and lifestyle factors such as light exposure, carbohydrate intake, exercise, and temperature variations like cold or heat exposure.
Beyond weight management, leptin affects brain health, sleep quality, and energy levels. Leptin is the hormone that regulates fecundity and fetal development in females. It also modulates immune T-cell function and maintain skeletal integrity in bones. Dysregulated leptin impairs the body’s ability to maintain energy homeostasis, leading to immunocompromise, fatigue, disrupted sleep, and a higher risk of neurodegenerative diseases. These effects are evident in daily life through struggles with hunger cues, poor energy levels, inadequate rest, and growth/development defects. Yet, GLP-1 drugs like Ozempic, Wegovy, and Mounjaro fail to address leptin resistance, a condition deeply tied to mitochondrial dysfunction. Instead, by artificially surging insulin, these drugs increase mitochondrial stress, elevate reactive oxygen species (ROS), and disrupt the delicate energy balance needed for proper leptin signaling and cellular repair.
Additionally, GLP-1 drugs may suppress appetite by targeting the brain’s hunger centers, but they do not resolve leptin resistance, which drives the problems GLP-1 agonists are trying to cover up. Without addressing the leptin resistance core issue, the underlying metabolic dysfunction persists. Ultimately, longevity is about addressing root causes, not quick fixes. GLP-1 drugs may offer temporary benefits but will absolutely increase risk of chronic metabolic disease, whilst increasing dependency on ongoing drug taking.
Natural Ways to Stimulate GLP-1 Without Drugs
GLP-1 is not just triggered by food, it is a whole-body environmental signaler, deeply tied to circadian biology. If you want to optimize it naturally, you must recreate the conditions under which humans evolved.
-
Food Timing and Quality: Distinct meals eaten during daylight hours, particularly those with protein-dense breakfasts, help amplify GLP-1 release. Pairing these meals with fiber-rich vegetables, fermented foods, and polyphenols from sources like green tea, berries, and cacao further supports enteroendocrine health by diversifying the microbiome. Healthy fats such as wild salmon, pastured eggs, olive oil, and ghee provide the structural components needed for GLP-1 receptor function. Importantly, GLP-1 secretion itself follows a circadian rhythm, with human studies showing higher postprandial GLP-1 responses during the biological day compared to night. This means that eating in alignment with natural light cycles enhances satiety signaling and glucose control. Conversely, disrupted sleep or exposure to artificial light at night alters both GLP-1 and insulin secretion, flattening their normal rhythms. Over time, this mismatch contributes to metabolic dysregulation, which is commonly observed in shift workers. Because meal timing entrains peripheral clocks, including those in L-cells, mistimed feeding such as late-night eating disrupts GLP-1 rhythmicity and impairs glucose tolerance.
-
Light and Darkness: Morning sunlight (especially infrared and UVA) stimulates gut–brain signaling through the vagus nerve and enteroendocrine cells. Darkness at night allows melatonin to rise, and melatonin directly supports GLP-1 secretion and gut repair. Artificial light at night suppresses this.
-
Temperature: Cold exposure activates brown adipose tissue, which improves GLP-1 secretion and insulin sensitivity. Heat (sauna or natural heat stress) also upregulates mitochondrial biogenesis and gut hormone signaling, further supporting GLP-1 rhythms.
-
Exercise and Movement: Post-meal walking, resistance training, and regular movement stimulate gut stretch receptors and vagal activity, enhancing GLP-1 release. Exercise also improves insulin sensitivity, creating a synergistic effect.
-
Breathing and Nervous System Regulation: Nasal breathing produces nitric oxide in the sinuses, which dilates vessels and improves metabolic signaling. Parasympathetic balance (via grounding, meditation, HRV-focused breathing) enhances vagal tone, making GLP-1’s signals more effective.
-
Hydration: Adequate water intake stretches gut mechanoreceptors, stimulating GLP-1. Structured water made by mitochondria (through light-driven OxPhos) adds an even deeper layer of hydration, critical for gut–brain hormonal communication.
-
Supplements and Nutrients: Vitamin D, magnesium, selenium, and B12 status are all linked to GLP-1 efficiency. Polyphenols and amino acids like arginine further support nitric oxide and gut hormone release.

When you integrate light, dark, food timing, temperature stress, and nervous system regulation, GLP-1 flows naturally and sustainably, without the dependency of synthetic agonists.
References
-
Short-Term Sleep Deprivation With Nocturnal Light Exposure Alters Time-Dependent Glucagon-Like Peptide-1 and Insulin Secretion in Male Volunteers. Gil-Lozano M, Hunter PM, Behan LA, et al. American Journal of Physiology. Endocrinology and Metabolism. 2016;310(1):E41-50. doi:10.1152/ajpendo.00298.2015.
-
Circadian Secretion Rhythm of GLP-1 and Its Influencing Factors. Liu C, Liu Y, Xin Y, Wang Y. Frontiers in Endocrinology. 2022;13:991397. doi:10.3389/fendo.2022.991397.
-
Circadian Rhythms Disrupted by Light at Night and Mistimed Food Intake Alter Hormonal Rhythms and Metabolism. Meléndez-Fernández OH, Liu JA, Nelson RJ. International Journal of Molecular Sciences. 2023;24(4):3392. doi:10.3390/ijms24043392.
-
Circadian Mechanisms in Medicine. Allada R, Bass J. The New England Journal of Medicine. 2021;384(6):550-561. doi:10.1056/NEJMra1802337.
-
Circadian Regulation of Glucose, Lipid, and Energy Metabolism in Humans. Poggiogalle E, Jamshed H, Peterson CM. Metabolism: Clinical and Experimental. 2018;84:11-27. doi:10.1016/j.metabol.2017.11.017.
-
Circadian Adaptations to Meal Timing: Neuroendocrine Mechanisms. Patton DF, Mistlberger RE. Frontiers in Neuroscience. 2013;7:185. doi:10.3389/fnins.2013.00185.
What’s Behind the Real Reason Human Metabolism is Under Attack?
Over the past 30 years, human metabolism has been increasingly compromised by profound environmental changes, with indoor living emerging as one of the most significant shifts. Today, the average person spends over 90% of their time indoors, blocking consistent exposure to natural light, fresh air, and organic soundscapes. These natural stimuli have been replaced by artificial substitutes, most notably artificial visible light and artificial non-visible light (EMF), which have dramatically altered the epigenome and disrupted biochemical processes vital to metabolic health.
The Loss of Natural Light and Its Consequences
The absence of natural sunlight, especially the full spectrum of infrared and ultraviolet light, has profoundly impacted mitochondrial repair and renewal. Infrared light governs mitochondrial autophagy (cellular renewal), while ultraviolet light regulates apoptosis (programmed cell death). Without these key wavelengths, damaged cells persist, and healthy cells struggle to regenerate. Modern windows filter out ultraviolet and infrared light while allowing only visible light to pass through, exposing indoor occupants to an unnatural spectrum. This deficiency is further compounded by the dominance of artificial visible light from technology screens, LEDs, car headlights, and streetlights, which lack over 60% of the light spectrum naturally delivered by the sun.
When this artificial visible light is encountered after sunset, it is referred to as artificial light at night (ALAN). ALAN disrupts circadian rhythms, suppresses melatonin production, and interferes with fat metabolism and cellular repair processes essential for long-term health.
The Growing Burden of Artificial Non-Visible Light (EMF)
The proliferation of artificial non-visible light (EMF), including radiofrequency (RF) radiation from Wi-Fi, Bluetooth, and mobile networks; alternating current (AC) electric and magnetic fields from power lines and household wiring; dirty electricity; and low-level currents in the environment, has created a pervasive and invisible stressor on human health. Today’s homes, offices, schools, and cars are saturated with EMFs, with the average home now hosting 25 wireless devices.
This artificial non-visible light (EMF) disrupts the body’s natural light signaling systems in several ways:
-
Impairing brain alpha waves in the thalamus
-
Disrupting cellular calcium signaling
-
Generating excessive reactive oxygen species (ROS)
-
Interfering with mitochondrial energy production and signaling
These disruptions alter how the body perceives and processes natural light signals, creating a metabolic cascade that impacts hormones like leptin, insulin, and melatonin, each of which is tightly yoked to light exposure for regulation.
The Role of Photoreception and Vitamin A
The skin and eyes rely on photoreceptive pigments, such as melanin, and light-sensitive receptors, including melanopsin (blue light), neuropsin (UV light), and rhodopsin (green light), to regulate metabolic health. These receptors depend on vitamin A to capture and translate light into direct current (DC) electrical signals that fuel epigenetic signaling and energy metabolism. However, exposure to artificial visible light and artificial non-visible light (EMF) ionizes vitamin A, releasing it from its photoreceptor bond. This triggers oxidative stress and renders these receptors nonfunctional. Additionally, the coupled feedback loop between vitamins A and D means that as vitamin A becomes depleted, vitamin D levels also drop, weakening immune defenses and impairing mitochondrial repair processes.
The Impact of Circadian Mismatches
Modern lifestyles further exacerbate these challenges by introducing circadian mismatches, such as consuming food out of sync with natural light conditions or eating non-local and non-seasonal foods. These practices disrupt the body’s natural rhythms, impair melatonin production, and reduce mitochondrial function. The gut, the body’s third major photonic interface, is lined with photoreceptors, immune cells, and bacteria that respond to the light and water signatures of the foods we eat. When these signatures do not align with the environmental signals received by the skin and eyes, or worse, when food is consumed in darkness, the result is disrupted circadian alignment, impaired autophagy, and metabolic inefficiency.
The Role of Artificial Light and EMF Exposure
Both artificial visible light (ALAN after sunset) and artificial non-visible light (EMF) immediately impact metabolic processes:
-
ALAN suppresses melatonin production, disrupts sleep quality, and impairs mitochondrial repair.
-
EMFs increase blood glucose levels, drive insulin resistance, and alter hormonal feedback loops, even independent of diet.
The absence of natural infrared light in modern environments further compounds these effects. Infrared light, which constitutes over 50% of sunlight, plays a critical role in energizing water networks within the body and sustaining mitochondrial efficiency. Without it, biological systems lose energy, tissues swell, and metabolic processes become inefficient, a hallmark of conditions like leptin resistance and chronic inflammation.
Why GLP-1 Drugs Cannot Fix the Real Problem
While GLP-1 receptor agonists offer temporary metabolic relief, they cannot repair the foundational disruptions caused by artificial light (visible and non-visible) and circadian mismatches. Without addressing these underlying environmental and biological dysfunctions, metabolic flexibility remains impaired, leaving the body vulnerable to chronic disease.
By failing to realign human metabolism with natural environmental cues, GLP-1 drugs perpetuate the very cycle of dependency and dysfunction they are designed to mitigate.
Improving GLP-1 Through Mitochondrial Health
By addressing the underlying mitochondrial misfunction, the body can become more efficient at regulating glucose and fat metabolism, enhancing the effects of GLP-1. Improving mitochondrial function allows the body to use energy more efficiently, reduce insulin resistance, and restore proper leptin signaling, leading to more sustainable weight loss, deeper sleep and better metabolic health.
GLP-1 agonist medications as Longevity Drugs
It's important to note that microdosing GLP-1 can be a possible 'biohacking' way to improve things in certain patients to support a transition to a better environment and lifestyle in a more light powerful environment such within -30 to +30 degrees latitude. In no way is this medical advice, but noting that longevity doctors and forward thinking low-dose prescribers are beginning to use this for various outcomes. That being said, our takeaway here is that all this tells us is the mechanism is intact to support Leptin signalling as the primary circadian signaler and why it's so important to manage your light environment, such as with full spectrum UV-VIS-IR lighting in your indoor environments and at a very minimum bioSpectral's melanin infused blue light blocking glasses.
A Very Dangerous Side-Effect of GLP-1 Drugs: Oh and you know how they tell you to avoid eating 12 hours before surgery? Well if your on a GLP-1 Agonist drug like Ozempic, perhaps extend this to 24-36 hours due to the gastric slowing effects of these drugs. Anesthesiologists are now dealing with multiple patients per week vomiting while they are unconscious during their surgeries due to this issue, when they used to only see it once or twice a year! When your unconscious under a general anasthetic you do not have a gag reflex and hence you can choke on your own vomit and die as the fluid leaks into the lungs. Safety first people.
Conclusion
The real issue lies in a profound and cascading disruption of the human body's natural rhythms and signaling mechanisms. Mitochondrial dysfunction, driven by environmental mismatches in natural and artificial visible light exposure, and natural and artificial non-visible EMFs, and modern indoor living, undermines the intricate communication networks that sustain metabolic health. The body’s ability to read and respond to environmental cues has been systematically eroded, with photoreceptors rendered useless, vitamin A and D levels depleted, and oxidative stress unchecked. This disarray cascades into hormonal imbalances, leptin resistance, and impaired mitochondrial signaling, leading to insulin resistance, chronic inflammation, and systemic energy deficits. At its core, the reliance on synthetic interventions like GLP-1 agonists to address metabolic issues ignores the broader, systemic breakdown of these fundamental biological processes, leaving the body further confused, misaligned, and vulnerable to shorter lifespan and more time with chronic disease. If the root cause is addressed, this restores endogenously produced GLP-1 agonist function and no drugs are needed, creating true longevity within your human living system.


Disclaimer
The information on this site is provided by BioSpectral Systems for educational and informational purposes only. It is not intended to diagnose, treat, cure, or prevent any disease and has not been evaluated by the U.S. Food and Drug Administration or any other regulatory authority. Always consult a qualified healthcare professional before making any changes to your health regimen. By using this site, you acknowledge that you do so at your own discretion and agree that BioSpectral Systems, its affiliates, and contributors are not liable for any outcome resulting from the use of the information presented.
Share:
The Mouth-Brain Connection. A Smarter Approach to Pediatric Development
Guest post: Sandcast Blog by Travis Mewhirter